Today, May 5, 2023 is Postpartum Psychosis Awareness Day, launched by survivors of postpartum psychosis in 2021 to raise awareness about the most severe and devastating of perinatal mental health disorders. This is an opportunity to support mothers and families who have experienced postpartum psychosis, to increase awareness of postpartum psychosis, and to provide education to mothers, families, and health care providers.
For women who are struggling with perinatal mood and anxiety disorders, emergency support can be found here:
Postpartum Support International HelpLine: 1-800-944-4773
Maternal Mental Health Hotline: 1-833-9-HELP4MOMS (via text or phone)
Content warning: This article contains information on perinatal psychiatric disorders, including mentions of self-harm, suicide, and child maltreatment.
In January, we first learned about Lindsay Clancy, a mother from nearby Duxbury, Massachusetts, who was accused of killing her three young children. As is the case with such tragic and unimaginable events, there are so many questions about what happened. Many reports in the media, including interviews with family and friends, state that Ms. Clancy was suffering from postpartum depression or postpartum psychosis.
There is so much we don’t know about Lindsay Clancy’s history and the events leading up to the death of her children. We cannot speculate on what happened, but we can provide information for those who wish to understand more about postpartum psychiatric disorders. There is often confusion about postpartum psychiatric illness, and it is important for women, their families, and their health care providers to be able to know what is a normal response to childbirth and the challenges of taking care of a new baby and what is something that requires medical attention.
Postpartum Depression and Anxiety Disorders
Many, if not most, women may experience some emotional turbulence during the first two weeks after the birth of a child. This is what we call “baby blues”. Women with postpartum blues do not describe feeling depressed or down; they do report feeling more emotional or vulnerable and that they cry more easily. In contrast to what we see with other types of postpartum mood and anxiety disorders, women with the blues are able to function well and can tend to themselves and their baby. The blues are the most evident during the first week after delivery and typically do not last beyond two weeks, nor do they require any specific intervention other than support and reassurance.
About 15% of women suffer from some type of postpartum mood or anxiety disorder. For some women this may be their first experience with depression or anxiety; however, the majority of women with postpartum mood and anxiety disorders have experienced depression or anxiety prior to or during pregnancy. In contrast to the blues, the symptoms associated with these disorders are more severe, longer lasting, and may affect a woman’s ability to function.
Postpartum Depression – In contrast to the blues, postpartum depression or PPD is a more severe and more persistent mood episode. Symptoms of PPD include feeling sad or depressed, not being able to enjoy oneself, changes in appetite (usually loss of appetite), changes in sleep (usually problems falling asleep), and, less commonly, suicidal thoughts. Women with PPD are often troubled by guilty thoughts, that they are not good enough mothers or that they are not doing enough for their baby.
Anxiety symptoms often accompany PPD and sometimes overshadow the depressive symptoms. Most commonly, women report feeling anxious or tense all the time and find it difficult to relax; they obsess about the health and welfare of the baby, and often worry about bad things happening to the baby — for example, worrying that the baby might become ill or injured or may die. These worries may also extend to other loved ones, and women may find it difficult to be away from their loved ones, for fear that something may happen to them. This type of anxiety may also make it difficult for the mother to allow and to trust others to care for the baby. Anxiety symptoms may have a profound impact on sleep, so that, even when the baby is sleeping, the mother may remain hypervigilant and worried about her baby.
Many women have unwanted, intrusive, and sometimes disturbing, thoughts or images of causing harm to their infant. These thoughts are extremely distressing to the mother. However, postpartum intrusive thoughts of accidental harm to the infant are common, nearly universal, and more than half of mothers with PPD report unwanted thoughts of intentionally harming their infant. While the mother has absolutely no intention of acting on these thoughts, mothers often fear that they may somehow lose control. Thus, they often go to great lengths to ensure the safety of the baby and may not feel comfortable being alone with the baby. There is no evidence to indicate that these intrusive thoughts are associated with increased risk to the infant.
Postpartum Anxiety – Some women present primarily with anxiety symptoms rather than depression. Similar to what we see with PPD, these symptoms often focus on the health and safety of the baby. These anxieties are often triggered by a real event or concern, including complications at the time of delivery, problems with breastfeeding, or having a baby that is smaller in size. Intrusive thoughts about harm to the infant are common. Postpartum anxiety may be associated with decreased appetite, weight loss, and significant sleep disruption.
In this setting, some women may have panic attacks, where they suddenly experience intense physical symptoms, such as palpitations, chest pain, or shortness of breath.
Postpartum Obsessive-Compulsive Disorder (OCD) – Many women with OCD prior to pregnancy experience worsening of their OCD after delivery, and sometimes women have the first onset of OCD during the postpartum period. Obsessive thoughts and rituals may focus on fears of contamination; obsessions and rituals related to the health and safety of the infant are common. However, women with postpartum OCD may also have very distressing, obsessive thoughts and images of causing harm to their infant.
Postpartum Psychosis
Postpartum psychosis is very rare, occurring in about 1 out of every 1000 childbirths. Because many women with PP psychosis have suicidal thoughts or behaviors that may compromise their ability to care for their baby, PP psychosis is a psychiatric emergency that requires immediate attention.
Risk Factors: While some women have no history of psychiatric illness, about 75% of women with postpartum psychosis have a history of bipolar disorder, or less commonly schizoaffective disorder or schizophrenia. Many women who have postpartum psychosis have a family history of postpartum psychosis or bipolar disorder.
Onset: Postpartum psychosis usually emerges quite rapidly over the course of a few days, representing a dramatic change in mood and behavior. Typically postpartum psychosis begins within the first two weeks after childbirth; rarely women present with psychotic symptoms after the first postpartum month.
Symptoms: Women with postpartum psychosis present with a range of symptoms that are most consistent with a mixed or manic affective episode as seen in individuals with bipolar disorder. There is, however, no “classic” presentation; some women may have very apparent symptoms, while others may have more subtle and less visible symptoms. In addition, It may also be difficult to recognize postpartum psychosis because the symptoms may have a waxing and waning or transitory quality. The full range of symptoms may not be obvious at a single time point or at the time of evaluation. Thus, it is important to consider, as part of a thorough evaluation, the impressions and observations of others – family, other health care providers — who are able to give a more longitudinal view of the illness.
Mood symptoms may precede the onset of psychotic symptoms. Women may present with mixed symptoms, including rapid fluctuations in mood, irritability, agitation, or severe anxiety. Less commonly, women present with hypomanic or manic symptoms: feeling overly elated and energetic, talking excitedly and rapidly, needing less sleep or inability to sleep, grandiosity or feeling that one has special qualities or abilities.
Sleep disruption: Most women with PP psychosis report the inability to fall asleep and stay asleep. Severe, persistent sleep problems may further complicate a woman’s ability to function and care for her infant.
Psychotic symptoms refer to delusions (false beliefs), hallucinations (hearing voices or having visions), and unusual, erratic, or disorganized behavior.
Delusional thoughts: Women with postpartum psychosis may have delusions of persecution and may believe somebody is trying to harm them or their baby, or they may believe that their baby is evil or gravely ill or not their baby at all. Women may have grandiose delusions about their baby’s abilities or their own powers. Delusions are sometimes religious in nature; many women with PP psychosis may believe that they are acting in accordance with God’s wishes. These delusional beliefs are not based in reality and may place the mother and her baby at risk, if the mother’s actions are guided by these delusional thoughts.
Paranoia, guardedness: Women with postpartum psychosis often have delusional thoughts that somebody is trying to hurt them or their baby. Thus, they may be suspicious of others, including family members, and may not openly express these fears. They may not allow others to care for the baby. They may not accept food or medicine from others because they may believe somebody is trying to control or poison them.
Ideas of reference: Women with PP psychosis may feel that certain events, objects, or experiences have a special and personal meaning. They may believe that a particular event or object is a sign, symbol, or message specifically meant for them. They may misinterpret casual events as having a personal significance, or they may feel that the media, for example, news reports or songs, is speaking directly to them. These messages may inform their behavior.
Hallucinations: Women with postpartum psychosis may experience a variety of hallucinations. These can include auditory hallucinations, such as hearing other people’s voices or talking or sounds that aren’t actually present, or visual hallucinations, where they see things that aren’t there. Some women may experience command auditory hallucinations which instruct them to harm themselves or their baby. Less commonly, women with postpartum psychosis may also experience olfactory or tactile hallucinations.
Agitation: Increased energy, restlessness, pacing, inability to sit still.
Erratic or disorganized behavior or speech: Psychotic symptoms may interfere with a woman’s ability to process information correctly, and this may result in strange or uncharacteristic behaviors. Speech may seem illogical or irrational. Women with PP psychosis sometimes appear to be confused or perplexed. This may affect their ability to appropriately feed and care for the baby. In this setting, a woman may not be able to respond appropriately to the baby’s cues and may have impaired judgment that compromises her ability to care for the baby.
Suicidal thoughts appear to be relatively common among women with PP psychosis, and women with PP psychosis are at high risk for suicide.
Thoughts of harming the baby: Women with PP psychosis may have thoughts of harming or killing their child. These thoughts reflect their delusional beliefs. Some mothers commit this act because they believe that the baby is gravely ill and the mother does not want the baby to suffer. Harm to the baby may occur when the mother is receiving messages from God or others that instruct her to kill her baby. It is important to note that these acts are extremely rare and that the vast majority of women who experience postpartum psychosis do not harm themselves or their children.
Suicidal Thoughts During the Postpartum Period
Suicidal thoughts may occur as a symptom of any of the psychiatric disorders described above. Suicidal thoughts may vary in intensity. A mother who is depressed may report passive suicidal ideation, stating that she wishes she were dead or thinks she would be better off dead, but she is not actively thinking about taking her own life. Less commonly, a woman may report active suicidal ideation and may be thinking about specific plans or methods to end her life. Suicidal thoughts are often accompanied by feelings of worthlessness and uselessness and the belief that the baby would be better off without their mother.
Although women are particularly vulnerable to mood and anxiety disorders during the postpartum period, suicide after the birth of a child is actually less common than at other times during a woman’s life. While suicidal ideation is commonly reported in women with PPD, women rarely act on these thoughts.
Suicidal ideation is especially concerning when it occurs within the context of postpartum psychosis. Because psychotic symptoms distort one’s perceptions and beliefs and interfere with one’s ability to make rational decisions, women with PP psychosis are at high risk for suicide.
Even when a woman reports that she has no desire or intention of acting on these suicidal thoughts, she should be evaluated by a medical professional. Suicidal ideation is never a normal event and must be viewed as a symptom of psychiatric illness.
Intrusive Thoughts or Psychotic Symptoms?
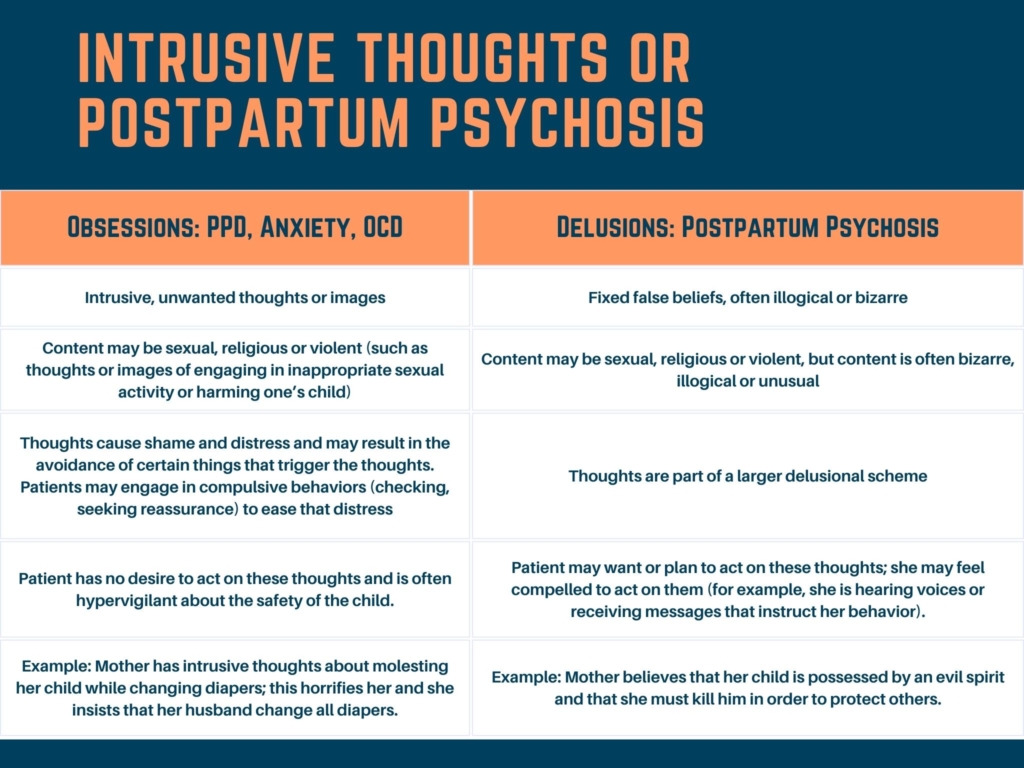
There is often confusion when it comes to distinguishing between intrusive thoughts and psychotic symptoms. Women with postpartum depression, anxiety, or OCD often have intrusive thoughts about accidental or intentional harm to their baby. These thoughts are unwanted, intrusive, and very distressing. When they occur as a symptom of postpartum depression or anxiety, the mother is very clear that she does not want to harm her infant and is very distressed or frightened by these thoughts. They are not part of a larger delusional pattern of thinking, and women with these thoughts usually go out of their way to make sure the baby is safe.
In contrast, when a woman with postpartum psychosis has thoughts of harming her child, it is in the context of her delusional thoughts.
This table is adapted from an excellent review article by Lauren Osborne and colleagues and helps to distinguish intrusive, anxious thoughts form delusional patterns of thinking:
Postpartum Psychosis is a Psychiatric Emergency
If it is suspected that a mother has postpartum psychosis, she should be evaluated by a medical professional emergently. Because rates of suicide and infanticide are high in this population, we generally recommend close observation and psychiatric hospitalization of women with PP psychosis.
For women who are struggling with perinatal mood and anxiety disorders, emergency support can be found here:
Postpartum Support International HelpLine: 1-800-944-4773
Maternal Mental Health Hotline: 1-833-9-HELP4MOMS (via text or phone)
The outcome described with respect to Lindsay Clancy is exceedingly rare. However, the tragedy has provided a springboard for discussion of postpartum psychiatric disorders, including the severe illness postpartum psychosis. Postpartum mood and anxiety disorders are common but are exquisitely treatable.








Leave A Comment